Abstract
Though many remain unaware of this, poverty, childhood abuse, and homelessness are not the only indicators of future drug misuse. Rather, people who grew up in stable, familial environments can often fall victim to addiction due to circumstances outside of their control. People who suffer from chronic pain are an example of this as many are forced to rely on narcotics and opioids in order to be able to get through their daily functions. Opioids are known for being extremely addictive substances capable of permanently altering a person’s neurobiology, however, in these circumstances, the benefits often outweigh the cost as people are now able to live a life with some semblance of normality.This paper reviews how addiction may occur in those who suffer from chronic pain, and where you can receive assistance if you are suffering from opioid addiction.
What is Chronic Pain?
Chronic pain is persistent pain that lasts 12 weeks or longer, most often occurring after recovery from injury and/or surgery. It may result in altered appetite, increased sensitivity to stress, other psychological deficits, and diminished mobility. It can occur anywhere on the body and is believed to be caused by damaged nerves. If you have suffered an injury or have undergone any surgical procedure and have been experiencing constant pain for over 12 weeks, you may be eligible to receive pain medication after visiting a clinician.

(Image Source: The Mesothelioma Center)
Chronic pain can also co-occur with certain health conditions. Examples include but are not limited to:
Endometriosis or uterine fibroids
Cancer
Chronic fatigue syndrome
Obesity
Multiple sclerosis
AIDS
Inflammatory bowel disease
Interstitial cystitis
(Image Source: The Good Body)
Chronic pain can be extremely emotionally taxing to deal with and can cause extreme changes in your current lifestyle. It is also recommended that besides visiting a clinician, a therapist would be an excellent investment. Other characteristics of chronic pain include muscle fatigue, muscle tension, exhaustion, and emotional frustration due to ongoing pain. Women, tobacco smokers, obese people, and those who have suffered from injury are most at risk. Treatments include muscle therapy, pain management rehab, and non-prescription drugs depending on the severity of the discomfort. Chronic pain can also lead to sleep disorders and severe depression, as depicted in the infographic provided by www.thegoodbody.com.
Responsible Use of Opioids
Doctors and physicians may deem that it is necessary to take opioid medication in order to deal with the side effects of debilitating pain. In this case, then it is alright to consume opioids with the directions provided by a qualified physician.
Prescription Opioid Medicines Include But Are Not Limited To:
• Hydrocodone (Vicodin®, Lortab®, Norco®) • Oxycodone (OxyContin®, Percocet®, Endocet®,)
• Morphine (MS Contin®, Kadian®, Oramorph SR®)
• Hydromorphone (Dilaudid®)
• Fentanyl (Duragesic®)
Opioids can also come from outside sources aside from healthcare providers. These include medications that are not prescribed to you, in other words, “street drugs”. These should never be taken in any scenario as you will not be aware of the ingredients that said drug is made from. It may be laced with drugs that are not opioids or counterfeit pills, such as fentanyl or carfentanil. Taking these can lead to extreme harm, overdose or death.
You should also ensure that you do not stray from your dosing plan. Your dosing plan was made in conjunction with your healthcare provider in order to treat your pain best. If you feel as though you are in need of a higher dosage, then you should consult the healthcare provider as you may be at risk of overdose if you take more medication than what was administered to you.
Physical Dependence vs Addiction
Repeated prescribed use inevitably leads to the development of tolerance and physical dependence, however, this does not necessarily mean addiction. The difference can be difficult to understand as there is lingering discourse among physicians as to what differentiates the two, however, there are some established distinctions. According to addictioncenter.com “Addiction is marked by a change in behavior caused by the biochemical changes in the brain after continued substance abuse. Substance use becomes the main priority of the addict, regardless of the harm they may cause to themselves or others. Addiction causes people to act irrationally when they don’t have the substance they are addicted to in their system.”
Furthermore, addiction encompasses both mental and physical reliance on a given substance rather than just physical dependency. Mental reliance occurs when the use of a substance is a conditioned response to an emotion, action or event. Physical dependence refers to when the body becomes reliant on a given substance and effects of withdrawal occur. When the body begins to build a tolerance towards said substance is also a symptom of physical reliance. Repeated administration eventually leads to a decrease in opioid potency, thus the prescription of opioids long-term will lead to increasingly higher doses. However, addiction is still avoidable and is not always the predicted outcome when prescribed opioid medication, whereas physical dependency is nearly inevitable.
Mitigation Strategies To Avoid Addiction
According to the American Medical Association, only 3% to 19% of chronic pain sufferers struggle with addiction. While prescription opioids will eventually lead to developing a physical dependence, there is an important distinction between that and addiction which is described above. However, when prescribed opioids for pain relief there is always a risk. Because opioids trigger the release of endorphins, thus activating the brain's powerful reward systems, it’s easy to begin relying on them more extensively than what was recommended by your doctor. Below are a series of mitigation techniques that can be used to avoid addiction as described by health professionals, along with common myths concerning opioid use.
Opioids are the safest when used for three or four days in order to manage acute (short-lasting) pain, however, chronic pain sufferers do not have this luxury. The likelihood of developing an addiction is affected and governed by numerous factors, meaning no simple change in lifestyle or prescription is guaranteed to devoid you of the risk. For example, avoiding the consumption of a specific type of opioid or avoiding prescribing a type of opioid to certain patients, cannot be expected to mitigate the risk of addiction. Regular monitoring and reassessment give opportunities to medical professionals to reduce risks associated with long-term opioid use by allowing for the adjustment or discontinuation of certain patients' prescriptions. Said patients should only include those who are not receiving clear benefits or are partaking in behaviors that increase their chance of overdose (Ex. poor adherence to prescription, consumption of high doses of alcohol etc.)
Deaths from opioid overdose have nearly quadrupled within the last two decades. Non fatal overdoses are even more prevalent and the contributing factors to these rates can be divided by opioid type, dose, potency, and duration of action (how long opioids remain in the body's systems). Although the use of any opioid can lead to opioid overdose, the increased risk is associated with higher doses. The risk of overdose has also been linked to the usage of long-acting opioids such as methadone and oxycodone. Patients with a history of overdose, history of addiction to any substances, suicidal thoughts, health conditions relating to the respiratory system and concurrent prescription of any medication that has depressive effects on the respiratory system are associated with increased risk as well. The recommended mitigation strategies for health professionals in clinical settings are as follows.
Addiction risks should be assessed prior to the prescription of opioids. Emerging signs of addiction can be seen through regularly monitoring patients, such as a urinary drug test occurring every meeting.
Avoiding Suicide As A Last Result
Co-occurring suicidal thoughts and chronic pain arenot rare, with evidence suggesting that nearly 20% of chronic pain sufferers are affected by this. As of now, the only sociodemographic associated with increased risk of suicidality in individuals with chronic pain would be those who are disabled and/or unemployed. A family history of depression along with harmful habits such as drinking or smoking are also identified as general risk factors. Co-occurrence of chronic pain conditions, sleep problems and more frequent intermittent pain are all found to be predictors of suicide as well. Thankfully a large number of these factors can mitigated through targeted intervention, highlighting a need for assessment of chronic pain patients who are at most risk, while also incorporating a suicide prevention component into pain management programs. Reaching out to someone (ie. a family member, nurse, spiritual leader, social worker, ortherapist) and prioritizing self-care and support are both great methods of healing. Reaching out to a suicide hotline can also be another great option as the freedom of anonymity can be a great relief.
However, the most effective method of avoiding suicide in chronic pain patients would be access to pain medication. For many, the main reason why suicide is looked
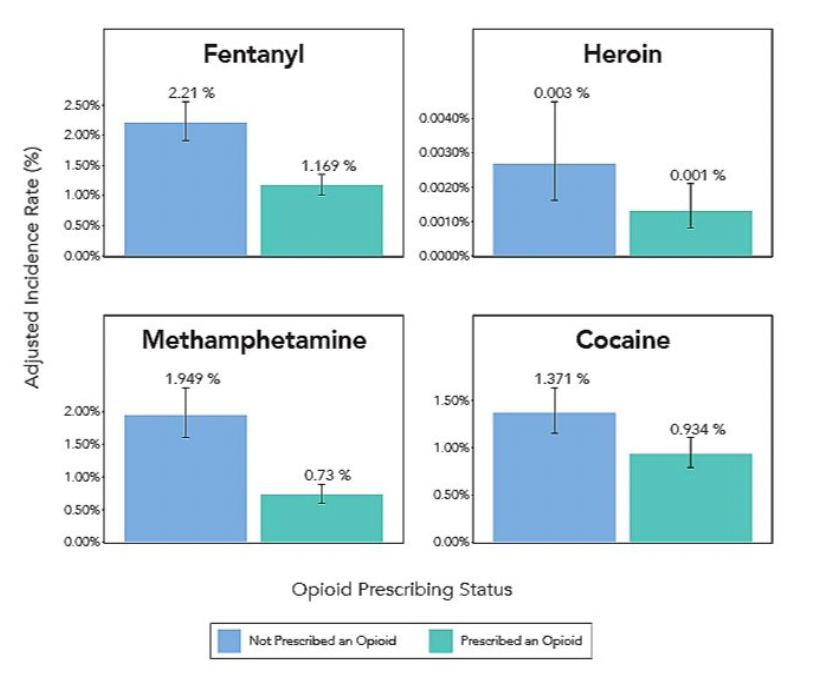
at as a viable alternative to living is to escape the agony that can accompany chronic pain. Thus prescription opioid medication can be considered the number one mitigation strategy to avoiding suicide. Interestingly enough according to a study conducted by Millennium Health, it appears that legal access to pain medication not only decreases risk of suicide, but also decreases substance abuse rates. However, who has access to these medications is heavily impacted by the DEA (Drug Enforcement Administration). The agency is primarily responsible for the enforcement and prevention of the abuse of illicit substances.
The Suicide Prevention Resource Center (SPRC) provides a virtual learning lab designed to build communities and provide more effective prevention efforts. The center also includes prevention methods in specific settings such as schools, college campuses or Native American and Alaskan Native Communities.
Website: Suicide Prevention Resource Center
SAMHSA Point of Contact: Brandon.Johnson1@samhsa.hhs.gov
Citation:
(Cover Image Source: The Minded Institute)
Risk Factors for Suicide among People with Chronic Pain - SPRC. https://www.sprc.org/system/files/private/event-training/handout-1_risk-factors-for-suicide-among-people-with-chronic-pain_508compliant.pdf.
“How Chronic Pain Can Lead to Addiction Issues.” Henry Ford Health - Detroit, MI, https://www.henryford.com/blog/2021/07/how-your-chronic-pain-can-lead-to-addiction-issues.
Opioid Abuse in Chronic Pain — Misconceptions and Mitigation Strategies. https://www.nejm.org/doi/full/10.1056/NEJMra1507771.
Substance Abuse and Mental Health Services Administration. https://store.samhsa.gov/sites/default/files/d7/priv/sma13-4671.pdf.
“Living with Pain Resources.” International Association for the Study of Pain (IASP), 23 Feb. 2022, https://www.iasp-pain.org/resources/living-with-pain/.
Sana LakeSana Lake Recovery Center is a Joint Commission Accredited addiction treatment program. We offer a safe and trustworthy facility for people struggling with substance abuse. “The Relationship between Chronic Pain and Addiction.” Sana Lake Recovery Center, 27 June 2022, https://sanalake.com/whats-the-relationship-between-chronic-pain-and-addiction/.
Hydrochlorothiazide: Basics, Side Effects & Reviews - Goodrx. https://www.goodrx.com/hydrochlorothiazide/what-is.
M;, Racine. “Chronic Pain and Suicide Risk: A Comprehensive Review.” Progress in Neuro-Psychopharmacology & Biological Psychiatry, U.S. National Library of Medicine, https://pubmed.ncbi.nlm.nih.gov/28847525/.
Anson, Pat. “Drug Tests Show Pain Patients on Opioids Less Likely to Use Illicit Drugs.” Pain News Network, Pain News Network, 10 Sept. 2022, https://www.painnewsnetwork.org/stories/2022/9/9/drug-tests-show-pain-patients-on-rx-opioids-less-likely-to-use-illicit-drugs.

Comments